S.I. No. 685/2016 - Medical Council Rules in Respect of the Duties of Council in Relation to Medical Education and Training (Section 88 of the Medical Practitioners Act 2007).
Notice of the making of this Statutory Instrument was published in | ||
“Iris Oifigiúil” of 31st March, 2017. | ||
| ||
Rule 1 | ||
The relevant criteria to be applied in respect of Section 88 (2)(a)(i)(I) of the Medical Practitioners Act 2007 (“the Act”) are as follows: | ||
1. The programme must be delivered by a body approved by the Medical Council under section 88(2)(a)(i)(II) as a body which may deliver a programme of basic medical education and training. | ||
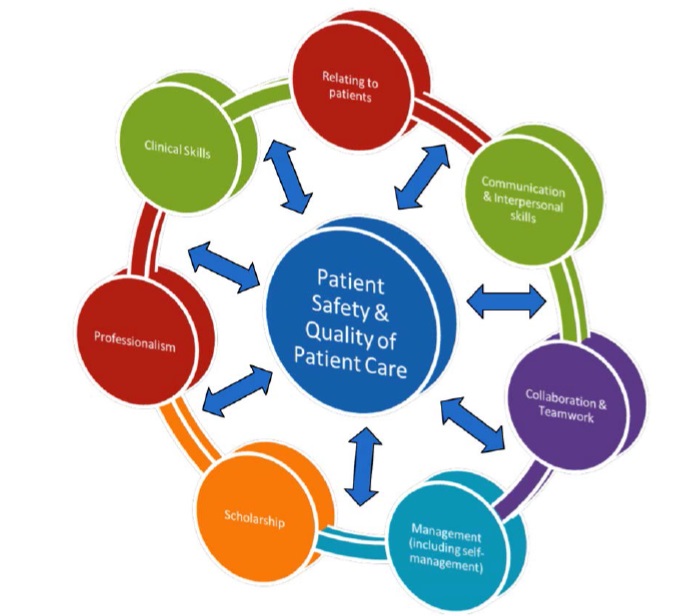
2. The programme will be required to demonstrate that it incorporates the Medical Council’s ‘Eight Domains of Good Professional Practice’, namely | ||
1. Patient Safety and Quality of Patient Care | ||
2. Relating to Patients | ||
3. Communication and Interpersonal Skills | ||
4. Collaboration and Teamwork | ||
5. Management (including Self Management) | ||
6. Scholarship | ||
7. Professionalism | ||
8. Clinical Skills | ||
and the Medical Council’s ‘Three Pillars of Good Professional Practice’, namely | ||
1. Partnership | ||
2. Practice | ||
3. Performance | ||
A copy of the ‘Eight Domains of Good Professional Practice’ is attached hereto at Appendix 1 and a copy of the ‘Three Pillars of Good Professional Practice’ is attached hereto at Appendix 2. | ||
3. A programme must comply with the basic requirements of the World Federation for Medical Education Global Standards for Quality Improvement in Medical Education: 2015 Revision to the extent that those standards apply to programmes of basic medical education and training. | ||
4. A programme must comply with the requirement in Article 24 of EU Directive 2005/36/EC for programmes of basic medical education. That Directive’s specification that programmes of basic medical education must include suitable clinical experience in hospitals under appropriate supervision will, at the discretion of the Medical Council, include suitable clinical experience in other clinical training sites under appropriate supervision. The 5,500 hours referred to in the Directive must be completed in a programme which is of a duration which is no less than four years. | ||
5. Approval of a programme will be for no longer than five years. Any significant alterations to the design and delivery of the programme, as approved, will require the prior approval of the Medical Council. | ||
6. Approved bodies will be required to submit annual declarations in respect of approved programmes. | ||
7. Failure to comply with any of the above may result in the withdrawal of approval. | ||
Rule 2 | ||
The relevant criteria to be applied in respect of Sections 88 (2)(a)(i)(II) and 88 (2)(a)(ii) of the Medical Practitioners Act 2007 (“the Act”) are as follows. | ||
1. A body must have been determined to be a college or university per the Universities Act 1997 . | ||
2. A body must comply with the basic requirements of the World Federation for Medical Education Global Standards for Quality Improvement in Medical Education: 2015 Revision to the extent that those standards apply to bodies which may deliver programmes of basic medical education and training. | ||
3. Approval of a body will be for no longer than five years. Any significant alterations to the status and/or structure of the body, as approved, will require the prior approval of the Medical Council. | ||
4. Failure to comply with any of the above may result in the withdrawal of approval. | ||
Rule 3 | ||
The relevant criteria to be applied in respect of Section 88(3)(a) of the Medical Practitioners Act 2007 (“the Act”) are as follows: | ||
1. The number of intern training posts to be specified by the Medical Council will depend on the extent to which the HSE in their proposal confirm that the posts identified in that proposal are part of a structured intern training programme organised through an Intern Training Network, which has clear educational objectives, measurable progression in ability, and externally validated assessment and which provides basic medical training leading to a certificate of experience that satisfies the requirement of Article 24 of Directive 2005/36/EC for this training to be provided by, or under the supervision of, a university. The posts must have designated educational trainer(s), each of whom must hold specialist division registration with the Medical Council. | ||
2. An intern training post: | ||
(a) Must comprise a minimum aggregate period of twelve months (comprising a minimum aggregate period of 1,500 hours of basic medical training leading to a certificate of experience) of which at least three months must be spent in Medicine in general and three months in Surgery in general | ||
(b) May include a rotation or rotations of not more than four months in one or more of the following specialties and not include rotations at all outside of these specialties: | ||
• Emergency Medicine | ||
• General Practice | ||
• Obstetrics and Gynaecology | ||
• Paediatrics | ||
• Psychiatry | ||
• Anaesthesia (to include perioperative medicine) | ||
• Radiology | ||
(c) Must not include any one rotation of less than two months | ||
Rule 4 | ||
1. The relevant criteria to be applied in respect of Section 88 (4)(a) of the Medical Practitioners Act 2007 (“the Act”) are as follows: | ||
(a) The post must be approved by a body approved by the Medical Council under section 89(3)(a)(ii) of the Act. | ||
(b) The post must be part of a programme approved by the Medical Council under section 89(3)(a)(i). | ||
| ||
The following rules are revoked: | ||
1. Medical Council Rules in respect of the duties of Council in relation to Medical Education and Training ( Section 88 of the Medical Practitioners Act 2007 ) commenced on 21st July 2010 (S.I. No. 528/2010). | ||
2. Medical Council Rules in respect of the duties of Council in relation to Medical Education and Training ( Section 88 of the Medical Practitioners Act 2007 ) commenced on 12th December 2012 (S.I. No. 588/2012). | ||
| ||
These Rules will commence on the 14th day of December 2016. | ||
| ||
| ||
| ||
Appendix 1 | ||
Eight Domains of Good Professional Practice | ||
| ||
| ||
Eight Domains of Good Professional Practice | ||
Patient Safety and Quality of Patient Care | ||
Patient safety and quality of patient care should be at the core of the health service delivery that a doctor provides. A doctor needs to be accountable to their professional body, to the organisation in which they work, to the Medical Council and to their patients thereby ensuring the patients whom they serve receive the best possible care. | ||
Relating to Patients | ||
Good medical practice is based on a relationship of trust between doctors and society and involves a partnership between patient and doctor that is based on mutual respect, confidentiality, honesty, responsibility and accountability. | ||
Communication and Interpersonal Skills | ||
Medical practitioners must demonstrate effective interpersonal communication skills. This enables the exchange of information, and allows for effective collaboration with patients, their families and also with clinical and non-clinical colleagues and the broader public. | ||
Collaboration and Teamwork | ||
Medical practitioners must co-operate with colleagues and work effectively with healthcare professionals from other disciplines and teams. He/she should ensure that there are clear lines of communication and systems of accountability in place among team members to protect patients. | ||
Management (including Self Management) | ||
A medical practitioner must understand how working in the health care system, delivering patient care and how other professional and personal activities affect other healthcare professionals, the healthcare system and wider society as a whole. | ||
Scholarship | ||
Medical practitioners must systematically acquire, understand and demonstrate the substantial body of knowledge that is at the forefront of the field of learning in their specialty, as part of a continuum of lifelong learning. They must also search for the best information and evidence to guide their professional practice. | ||
Professionalism | ||
Medical practitioners must demonstrate a commitment to fulfilling professional responsibilities by adhering to the standards specified in the Medical Council’s “Guide to Professional Conduct and Ethics for Registered Medical Practitioners”. | ||
Clinical Skills | ||
The maintenance of Professional Competence in the clinical skills domain is clearly specialty-specific and standards should be set by the relevant Post-Graduate Training Body according to international benchmarks. | ||
Appendix 2 | ||
Three Pillars of Good Professional Practice | ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
EXPLANATORY NOTE | ||
(This note is not part of the Instrument and does not purport to be a legal interpretation.) | ||
Any reference to the Medical Practitioners Act 2007 includes the amendment of that Act by the Health (Miscellaneous Provisions) Act 2007 , the Medical Practitioners (Amendment) Act 2011 and any subsequent amendments. | ||
The Definition of EU Directive 2005/36/EC of the European Parliament and of the Council which is provided for in Section 2 of the Medical Practitioners Act 2007 includes the Amendment of that Directive by Council Directive 2006/100/EC and any subsequent amendments. | ||
These rules were made by the Medical Council on 14th December 2016. | ||